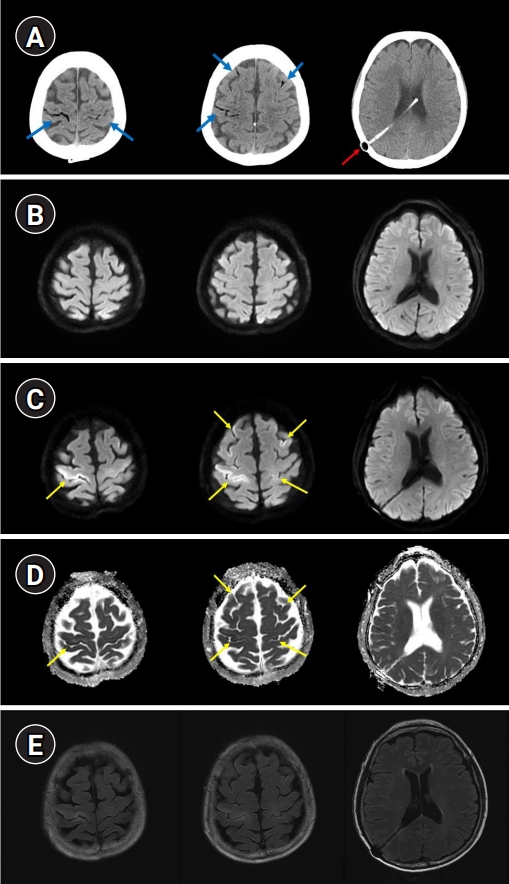
A 63-year-old woman had a sudden cardiac arrest while undergoing tooth scaling. After 4 minutes, the return of spontaneous circulation (ROSC) was achieved. She was stuporose, but other neurological examinations were within normal limits. The patient had a history of meningitis, and she had undergone ventriculoperitoneal shunt surgery for hydrocephalus in her 20s. Brain computed tomography performed immediately after ROSC showed cerebral air emboli (Fig. 1A). Brain magnetic resonance imaging (MRI) after 5 hours showed no acute lesions (Fig. 1B). Targeted temperature management was performed. Her consciousness improved to a drowsy state, but left hemiparesis was observed. Brain MRI performed on the 6th day showed gyriform infarction in both frontoparietal cortices that were consistent with air emboli (Fig. 1C-E).
Cerebral air embolism can lead to arterial and venous infarctions [1,2]. They can lead to blood flow obstruction and induce an inflammatory reaction with the breakdown of the blood-brain barrier [3]. In this case, the delayed cerebral infarction was detected by follow-up brain imaging. Cerebral venous air emboli can cause delayed cerebral infarction because the collateral circulation in the cerebral venous system allows for compensation. Even if the initial MRI is negative, repeated brain MRI may help detect cerebral infarctions caused by cerebral venous air emboli.