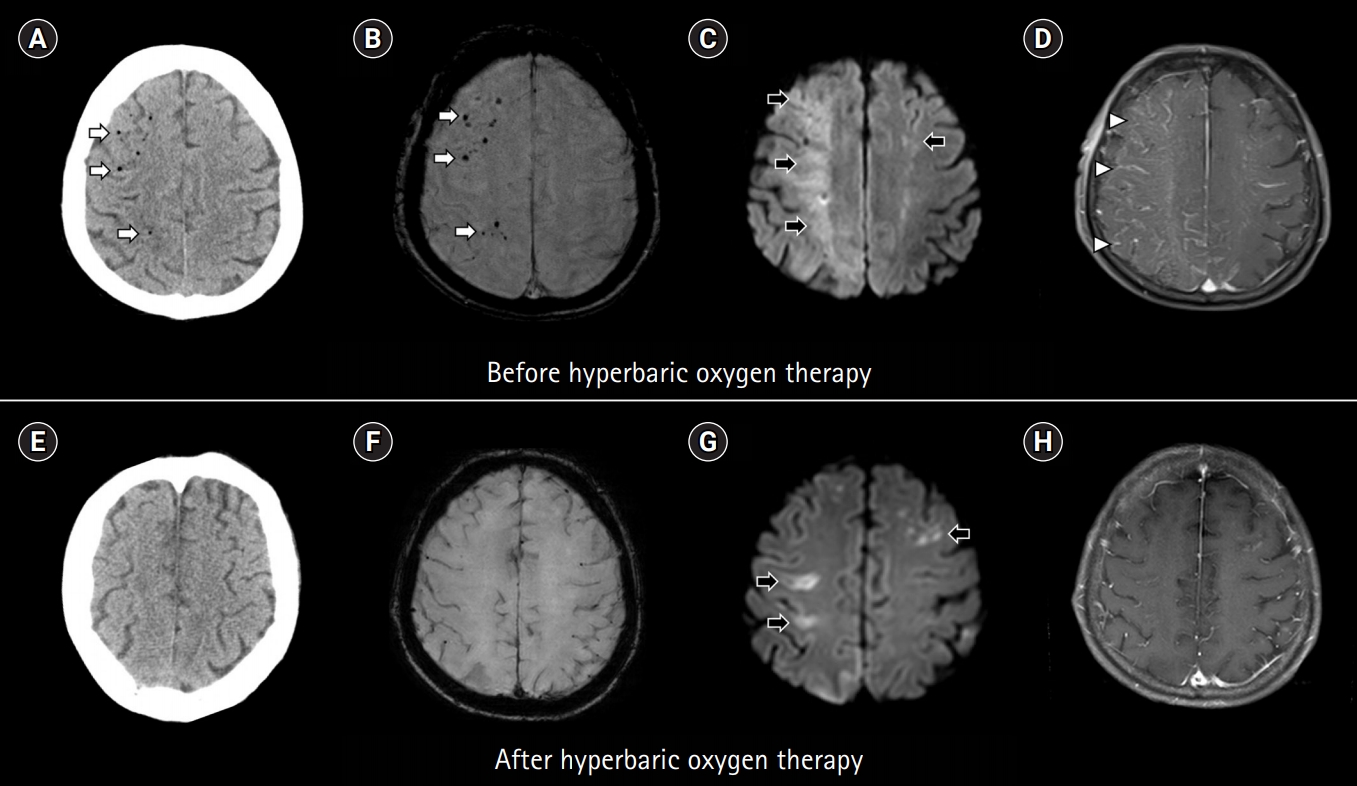
A 59-year-old man underwent endoscopic balloon dilation for esophageal stricture. Upon the completion of the procedure, he was observed to be stuporous and quadriplegic. Computed tomography (CT) of the brain revealed multiple air emboli (Fig. 1A). Magnetic resonance imaging (MRI) performed 45 minutes after symptom onset revealed multiple lesions showing signal loss on susceptibility-weighted imaging, high signal intensity on diffusion-weighted imaging, and diffuse enhancement on T1-weighted contrast-enhanced imaging, which were compatible with air emboli, hyperacute infarcts, and a disrupted blood-brain barrier, respectively (Fig. 1B-1D). Hyperbaric oxygen therapy (HBOT) was administered 80 minutes after MRI (targeting 3.0 atmospheric pressure for 2 hours). Follow-up CT performed 80 minutes after HBOT revealed disappearance of the air emboli (Fig. 1E). Follow-up MRI performed 5 days after HBOT also revealed a decrease in the resolution of previously documented findings (Fig. 1F-1H). Most of his neurological symptoms improved, except mild left hemiparesis.
This case indicates that MRI is a useful modality in diagnosing cerebral air embolism by documenting air emboli, hyperacute infarcts, and disruption of the bloodŌĆōbrain barrier [1-3]. HBOT may accelerate the disappearance of air emboli and promote the early resolution of ischemic lesions and reversal of the disrupted bloodŌĆōbrain barrier [4].