INTRODUCTION
After five successful clinical trials for mechanical thrombectomy have been published in 2015, endovascular treatment for acute ischemic stroke (AIS) caused by acute large-vessel occlusion (ALVO) in anterior circulation is now the standard of care for patients presenting within 6 hours of symptom onset [1-5]. However, this treatment option cannot be generalized like using intravenous (IV) tissue plasminogen activator (t-PA) in AIS. Many previous data have shown that roughly fewer than one-third of stroke centers are comprehensive stroke centers with on-site neurointerventionist [6]. Therefore, not all AIS patients with ALVO can be directly admitted to a comprehensive stroke center that can offer both IV thrombolysis and mechanical thrombectomy. To solve this problem, Drip-and-Ship (D-S) model using IV t-PA at the nearest hospital before being transferred into a comprehensive stroke center for mechanical thrombectomy has been proposed for AIS patients.
The critical problem of the D-S model is a longer process time by a time delay of inter-hospital transportation [7-10]. However, several reports after 2015 have shown a decrement of inter-hospital transportation due to better recognition of the importance of the process time after the publication of trials and a learning curve effect at several levels (such as advanced prehospital notification, cooperation between centers, and rapid response of neurointerventionist) [10,11]. The objective of this study was to investigate changes of inter-hospital transportation time calculated as image to door (ITD) time (from first image at primary hospital to arrival time at emergency room (ER) of a comprehensive stroke center) before and after 2015 in Busan metropolitan area, Korea.
METHODS
This was a retrospective observational study. It was approved by Dong-A University Hospital (DAUH) Institutional Review Board. For the purpose of this study, AIS patients with thrombolysis (IV t-PA and/or mechanical thrombectomy) under D-S or Ship-and-Drip (S-D) paradigm between January 2013 and December 2017 were identified from our stroke registry. DAUH is a tertiary teaching hospital located in the Busan metropolitan area (size, 765.64 km2; population, ~4 million). Our stroke center is a regional comprehensive stroke center in the Busan metropolitan area supported by the Korean government. When the comprehensive stroke center was opened, an 8-bed stroke care unit was formed for the care of acute stroke patients. This unit contains a telemetry system for monitoring of blood pressure, pulse, respiration, and oxygenation. A multidisciplinary group developed stroke care pathways to guide the evaluation and treatment of each stroke subtype. Stroke treatment was generally administered according to a well-organized team approach, e.g., IV thrombolysis, endovascular treatment, hemicraniectomy, and carotid endarterectomy.
Our strategy for using IV t-PA is based on magnetic resonance imaging (MRI) in principle. Our door to image time is maintained within 23 minutes. In 2015, a hotline system (1899-0215 in conjunction with the Korean Emergency Medical Information System [KEMS; 119]) was implemented in our hospital for prehospital notification. The primary role of the KEMS is to connect a patient needing an emergency or operation in a community hospital with appropriate available hospital [12].
Critical pathway for hyperacute ischemic stroke
Our stroke critical pathway is based on CODE RED program [13], a kind of computerized physician order entry system that enables activation, communication, notification, entering predetermined standing order sets, and providing protocols and guidelines [11]. In our stroke code system, MRI is routinely performed to screen patients for thrombolytic therapy. However, when an immediate MRI is unavailable because it is being used for other patients, brain computed tomography (CT) is used for IV t-PA. It is administered according to the National Institute of Neurological Disorders and Stroke criteria [12]. For such cases, MRI was performed before mechanical thrombectomy.
Definition of time points
In this study, two time points were used to evaluate time intervals of D-S paradigm for thrombolysis as follows: ITD time and onset to puncture (OTP) time (from symptom onset to groin puncture time).
Statistical analysis
In this study, data of National Institute of Health Stroke Scale (NIHSS), ITD time, OTP time, and transfer distance for included patients from 2013 into 2017 were collected. These parameters are expressed as median (interquartile range [IQR]). Statistical analysis of the serial trend of above parameters compared to those in 2013 and 2014 were conducted by using Kruskal-Wallis test. A P value of less than 0.05 was considered statistically significant. All statistical analyses were carried out using the SPSS version 21.0 (IBM Corp., Armonk, NY, USA).
RESULTS
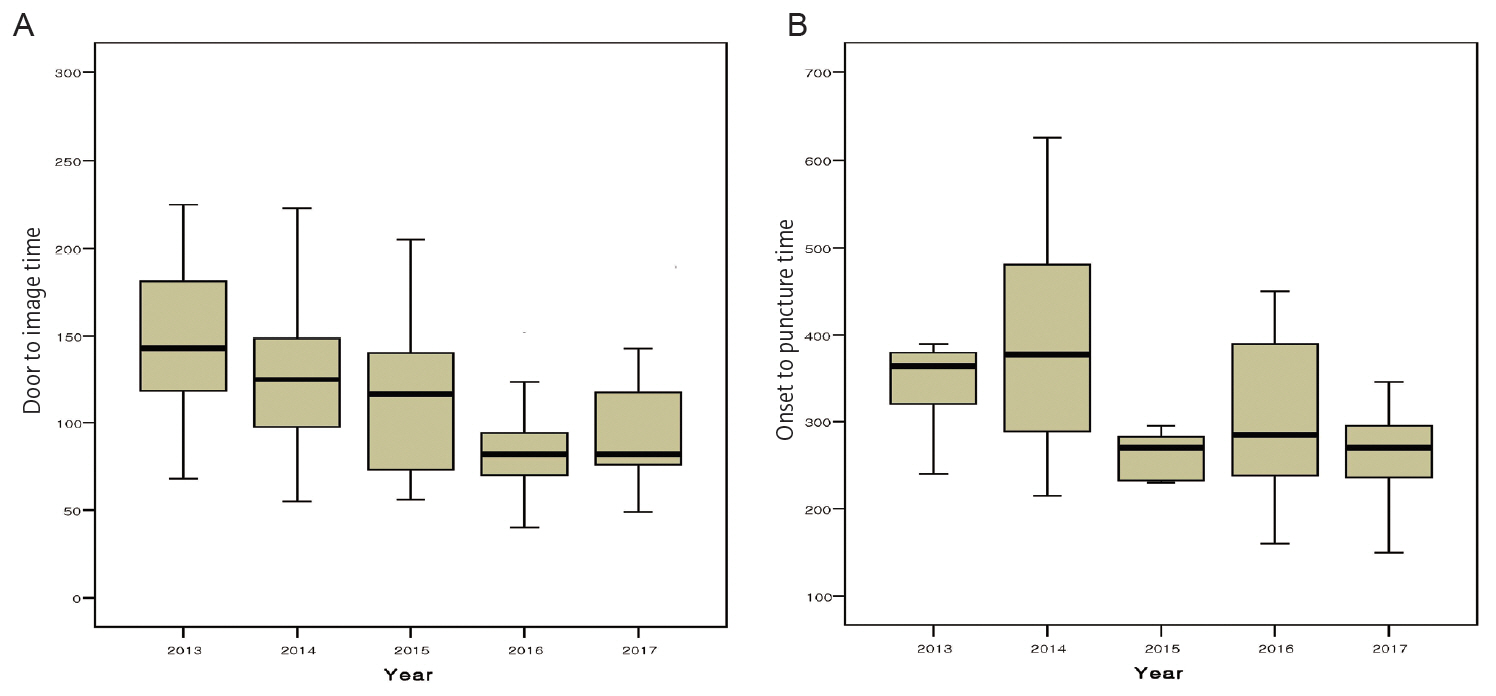
During the observation period, 806 patients received IV t-PA and/or mechanical thrombectomy. Among them, 225 subjects (27.9%) were treated under D-S or S-D paradigm. Of these 225 patients, 23 were excluded because of the lack of detailed data. Finally, 202 patients were enrolled in this study. Of these 202 patients, 73 were treated under D-S while 129 were treated under S-D. A total of 134 patients received IV t-PA only. Seventeen received mechanical thrombectomy only while 51 received mechanical thrombectomy after receiving IV t-PA. The median image to arrival time was 116 minutes (IQR, 92) in 2013. After 2015, the time interval gradually decreased. It was significantly (P<0.01) decreased to 85 minutes (IQR, 67) in 2017. The initial median neurologic severity measured by NIHSS was 9 (IQR, 10) in 2013. There was no difference in NIHSS during the observation period (Table 1, Fig. 1).
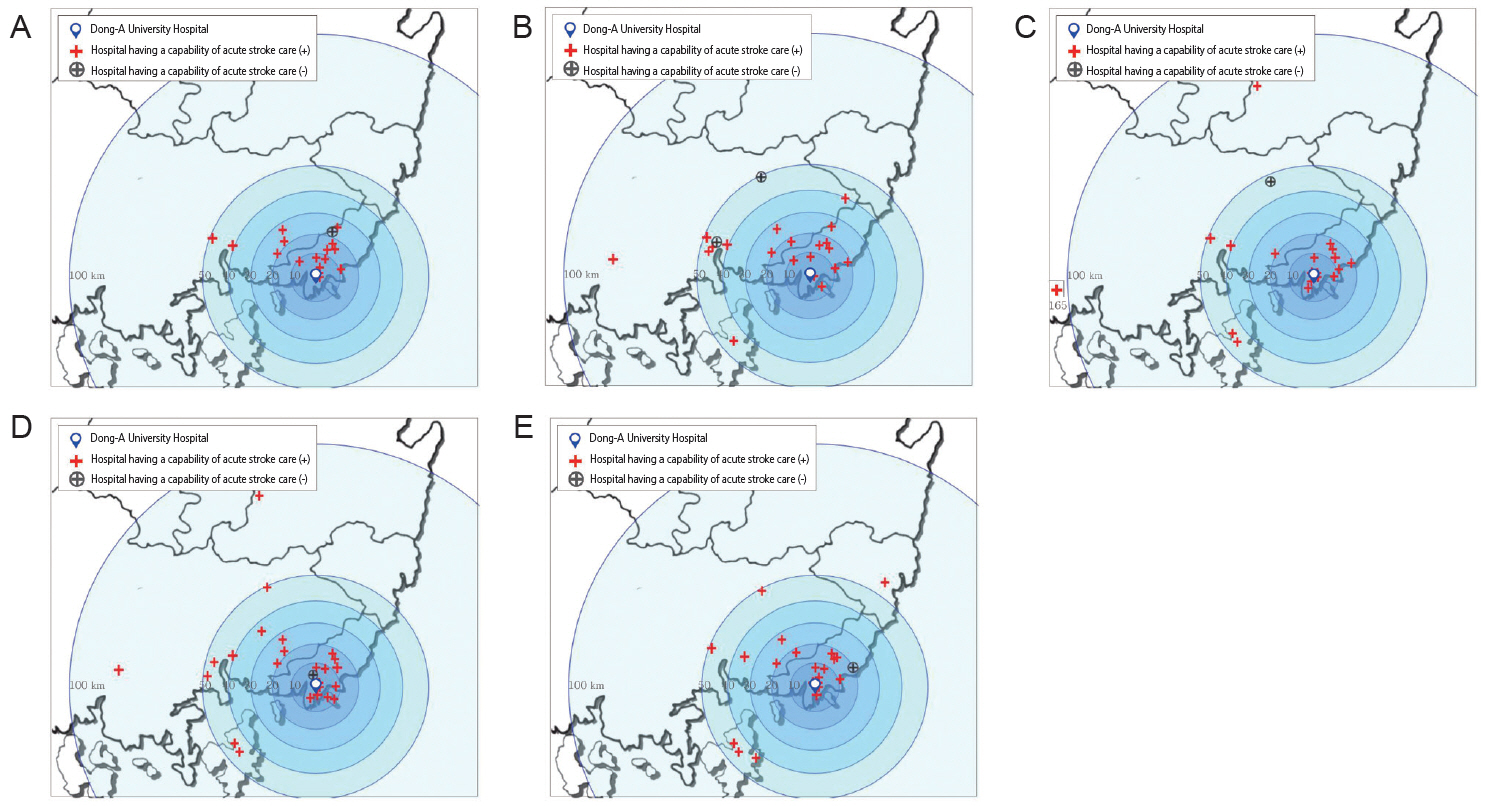
Regarding characteristics of hospitals from which acute stroke patients were transferred to our center, more than 95% of hospitals having their own stroke neurologist or neurosurgeon and Angio CT were capable of treating acute stroke. The median transfer distance was 25 km (IQR, 24) in 2013. It showed no significant difference during the observation period (Fig. 2).
Among 202 patients enrolled for this study, a total of 68 received mechanical thrombectomy during the observation period. In 2013, the median OTP time was 365 minutes (IQR, 97.5). It was significantly decreased to 270 minutes (IQR, 65) in 2015, 285 minutes (IQR, 189) in 2016, and 270 minutes (IQR, 72) in 2017 (P=0.03, Table 1, Fig. 1). After 90 days of thrombolysis, the rate of poor outcome (defined as modified Rankin scores of 3-6) was 54.3% in 2013, 66.7% in 2014, 52.9% in 2015, 57.7% in 2016, and 51.3% in 2017.
DISCUSSION
It is well-known that inter-hospital transfer time is the most important factor associated with treatment delay for mechanical thrombectomy [7-10]. Therefore, decreasing the time delay might be essential to achieve efficacious D-S paradigm for mechanical thrombectomy in our regional boundary of stroke care [14-18].
Transfer time from the first call to arriving at an ER of a hospital for Busan metropolitan area is about 25 minutes [19]. Such a short time from home to a neighboring ER makes our emergency medical service (EMS) paramedics unable to detect the presence of ALVO on EMS ambulance. Due to such problem, it is impossible to use the mothership paradigm for mechanical thrombectomy in Busan metropolitan area.
Busan metropolitan area has a unique pattern of D-S paradigm, showing more severe neurologic deficits at admission and much worse outcome after thrombolysis [12]. This result could be explained that many hospitals in Busan have their own stroke neurologist and their own Angio CT and/or MRI. Therefore, in our metropolitan area, almost all patients who received IV t-PA were initially treated by a stroke neurologist or neurosurgeon in a community hospital while only selected patients were transferred to our comprehensive stroke center due to the lack of mechanical thrombectomy or more intensive care after a phone consultation. In line with our previous data [12], the present study showed that more than 95% hospitals that sent patients to our center had capability for treating acute stroke. This pattern was similarly found in CRCS-K registry data in Korea showing that only patients with severe neurological deficits requiring further intensive care after t-PA administration were likely to be transferred to comprehensive stroke centers [20].
The inter-hospital transfer time calculated by ITD time was about 116 minutes in 2013 in the present study. This time interval was significantly delayed compared to previous reports in other countries showing 85 minutes of interhospital transfer time from primary stroke center to comprehensive stroke center [21,22]. Several factors might have limited rapid transfer of acute stroke patients between hospitals. First, there has been no governance to control transportation of stroke patients in Busan metropolitan area. Second, after deciding to transfer ALVO patients to a comprehensive stroke center, a substantial amount of time is needed for administrative procedures, release of medical records including hard copies of CT or MRI images, and checkout procedures at discharge. In fact, almost all time delays of inter-hospital transfer were caused by work-up procedure in a primary hospital [23,24]. Third, it was not easy for neighboring community hospitals to contact stroke physicians in our comprehensive stroke center.
In our stroke boundary, D-S or S-D paradigm for patients undergoing thrombolysis has already been voluntarily performed by neighboring hospitals and our comprehensive stroke center from 2009 [12,19,25]. To make ensure a prenotification between neighboring hospitals and our comprehensive stroke center, we have opened our individual mobile phones to neighboring hospitals in our stroke region. Since 2015, we have used the hotline number that is connected to neighboring hospitals and EMS paramedics in Busan metropolitan area [25]. As a consequence of above efforts, the proportion of D-S or S-D paradigm was 27.9% during the observation period in our center. This proportion is twice higher than those in other similar comprehensive stroke centers in CRCS-K registry [20]. Particularly, there were no significant differences in transportation time of stroke patients to our comprehensive stroke center from participating hospitals between our previous 2009 study [12] and the present data. Sun and colleagues [26] have found that the more often patients are transferred by the same hospital to a comprehensive stroke center, the more often transfer time interval is decreased. The significant decrement of inter-hospital transfer time in this study might be due to combined results of efficient pre-hospital notification by using our hot line system and increased recognition of rapid transportation for acute stroke patients with a learning curve on how to effectively transfer AIS patients into comprehensive stroke center after 2015 with five successful mechanical thrombectomy trials.
The median OTP time was also significantly decreased from 365 minutes in 2013 to 270 minutes in 2017 in the present study. This beneficial effect was mainly due to a significant reduction in inter-hospital transfer time. Prehospital notification by a stroke physician in neighboring community hospitals might have decreased intra-hospital processing time for mechanical thrombectomy in our comprehensive stroke center. In MR CLEAN trial [23], an increased time to arrival at the ER in transferred patients was clearly associated with a decrease in the following time to groin puncture. This paradoxical effect is likely caused by the fact that a comprehensive stroke center is pre-notified before arrival at the ER, making it possible to reduce the door to puncture time. However, we did not show this beneficial effect by a pre-hospital notification on D-S paradigm in detail.
Like several regions such as Paris [10], Frankfurt [11], and several cities in Holland [23] having geographic proximity that achieved effective organized stroke network based on D-S paradigm, this strategy might be applied in Busan for mechanical thrombectomy. Reducing transportation time to a comprehensive stroke center might be essential for successful D-S paradigm. In this sense, significant shortening of ITD time could be an important cornerstone to build up an effective organized stroke center in our stroke boundary. Although ITD time was significantly decreased to 85 minutes in 2017, it was more than 30 minutes longer than that of previous reports [10,11,23] with organized stroke network in several European countries. This difference might be associated with different characteristics of medical systems. Unlike European countries, more than 70% of hospitals in Korea belong to the private sector. This kind of difference might have influenced the delay of inter-hospital transfer time in Busan metropolitan area. More detailed investigation is needed to test this hypothesis in the future.
This study has several limitations. First, this was a retrospective study. Second, we were not able to obtain the door to needle time in patients treated under the D-S paradigm.
CONCLUSION
The inter-hospital transfer time was significantly decreased after 2015 in our stroke boundary of Busan metropolitan area. Our results implicated that many hospitals in our stroke region might have recognized the importance of rapid transportation for acute ischemic stroke after 2015. Based on this achievement, we should be able to build up an organized stroke system having a form of D-S paradigm in the future.